Reading Room Assistant
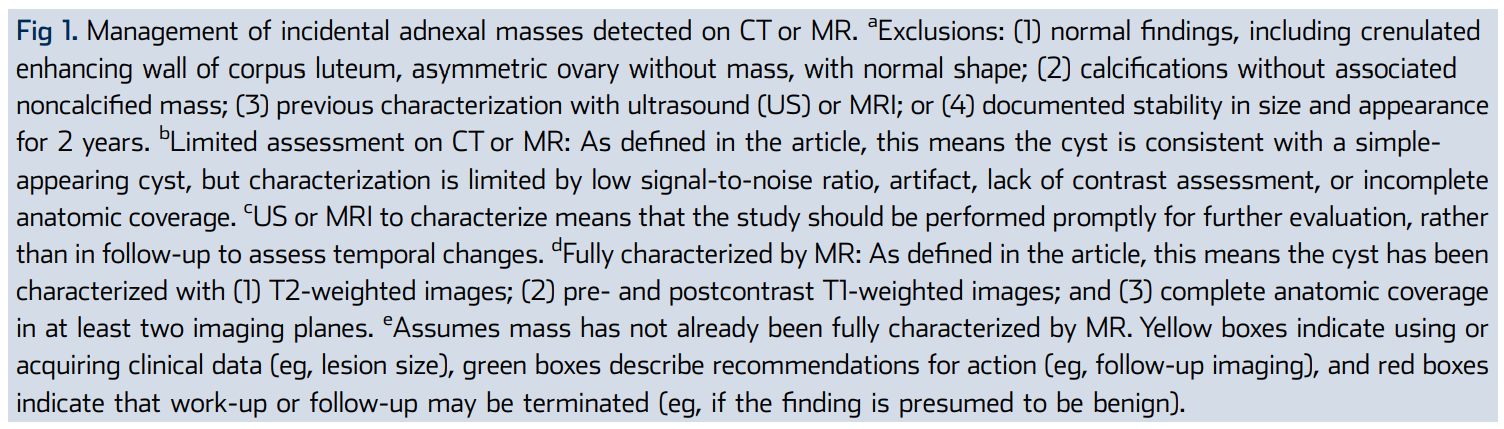
- Adnexa ACR
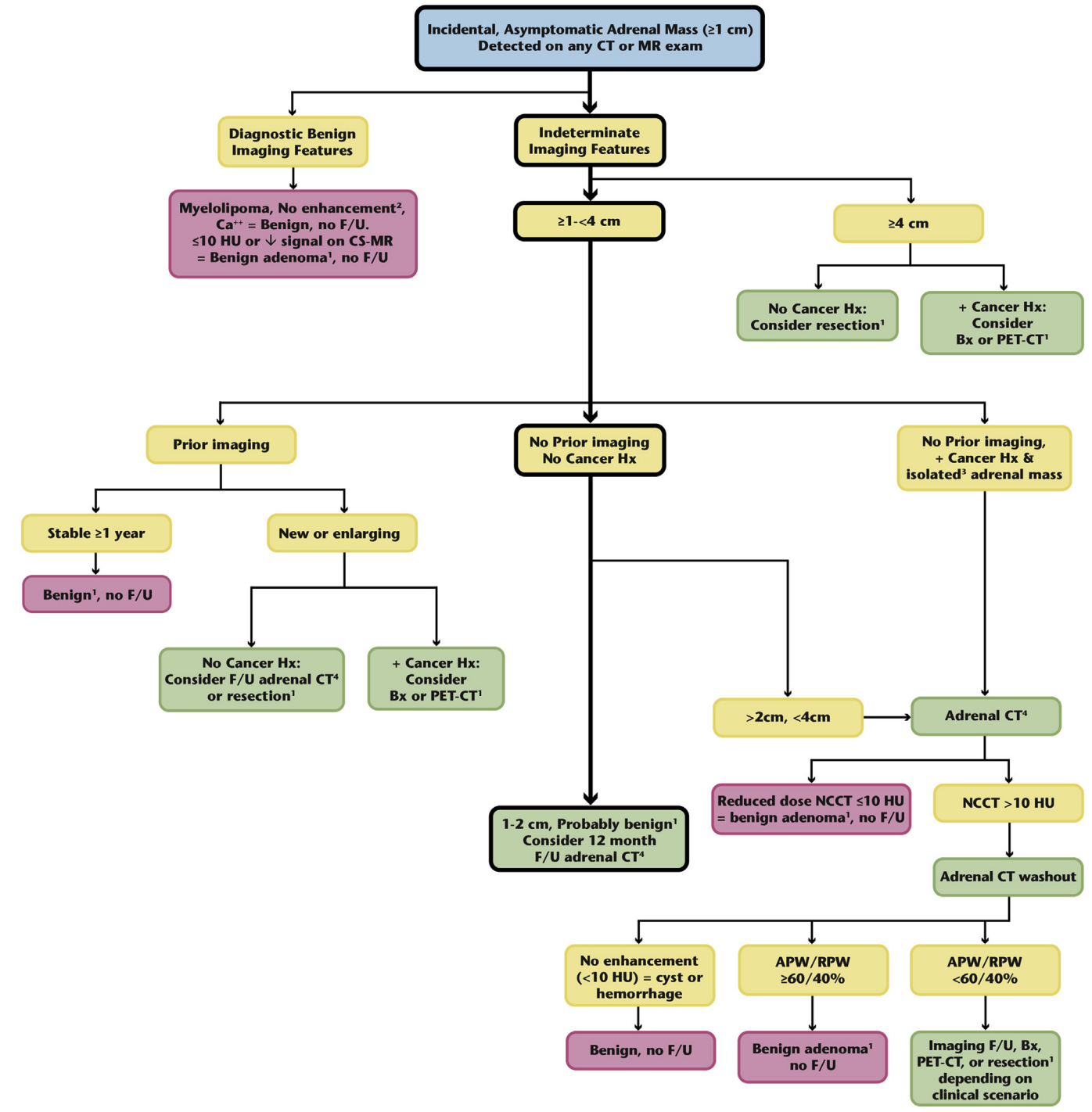
- Adrenal ACR
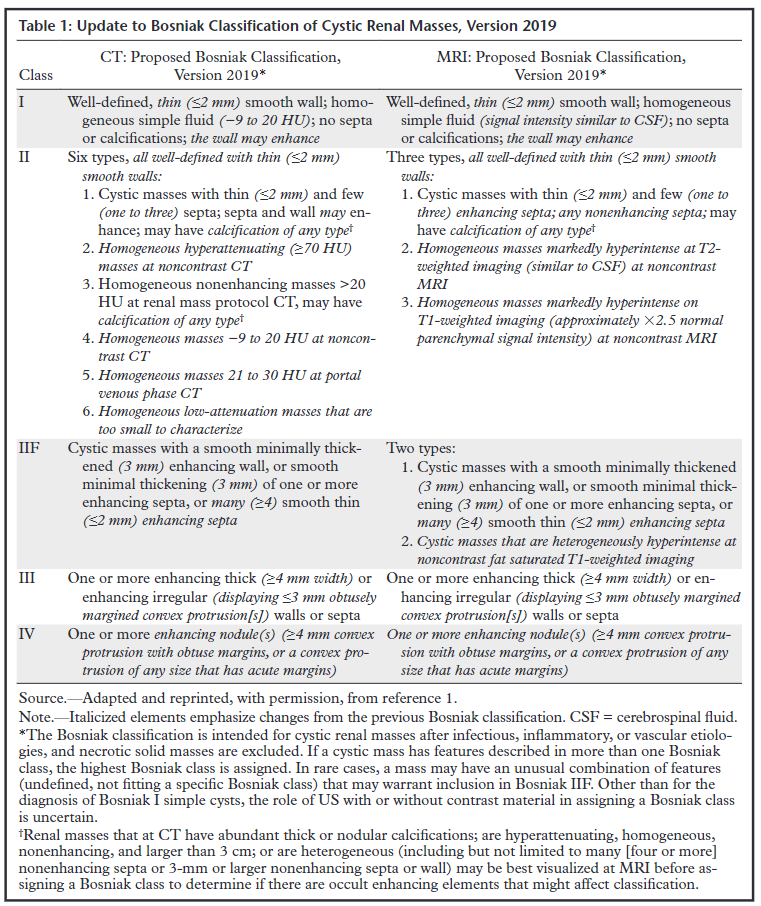
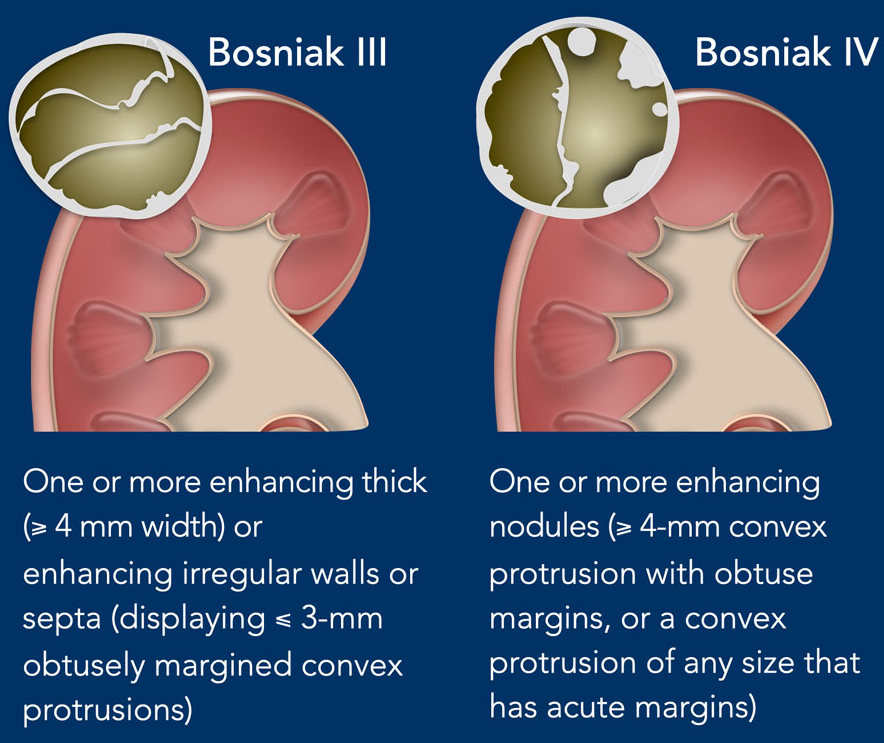
- Bosniak
- Gallbladder Polyp
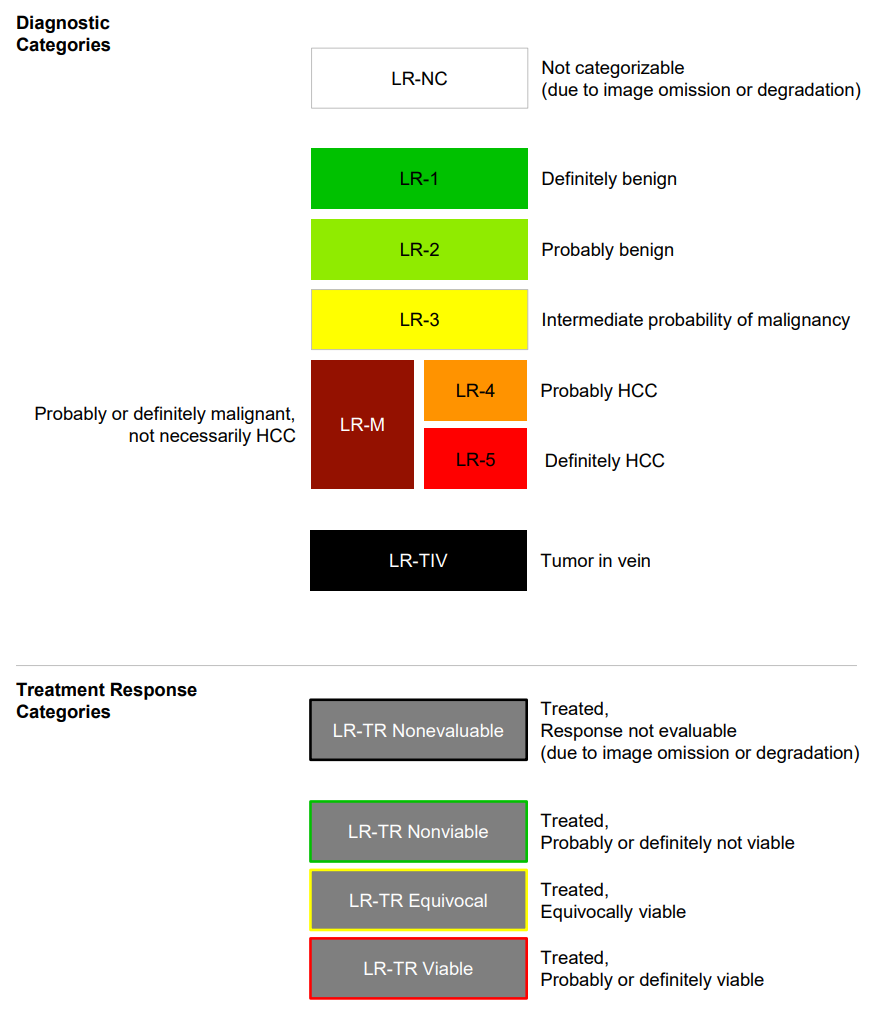
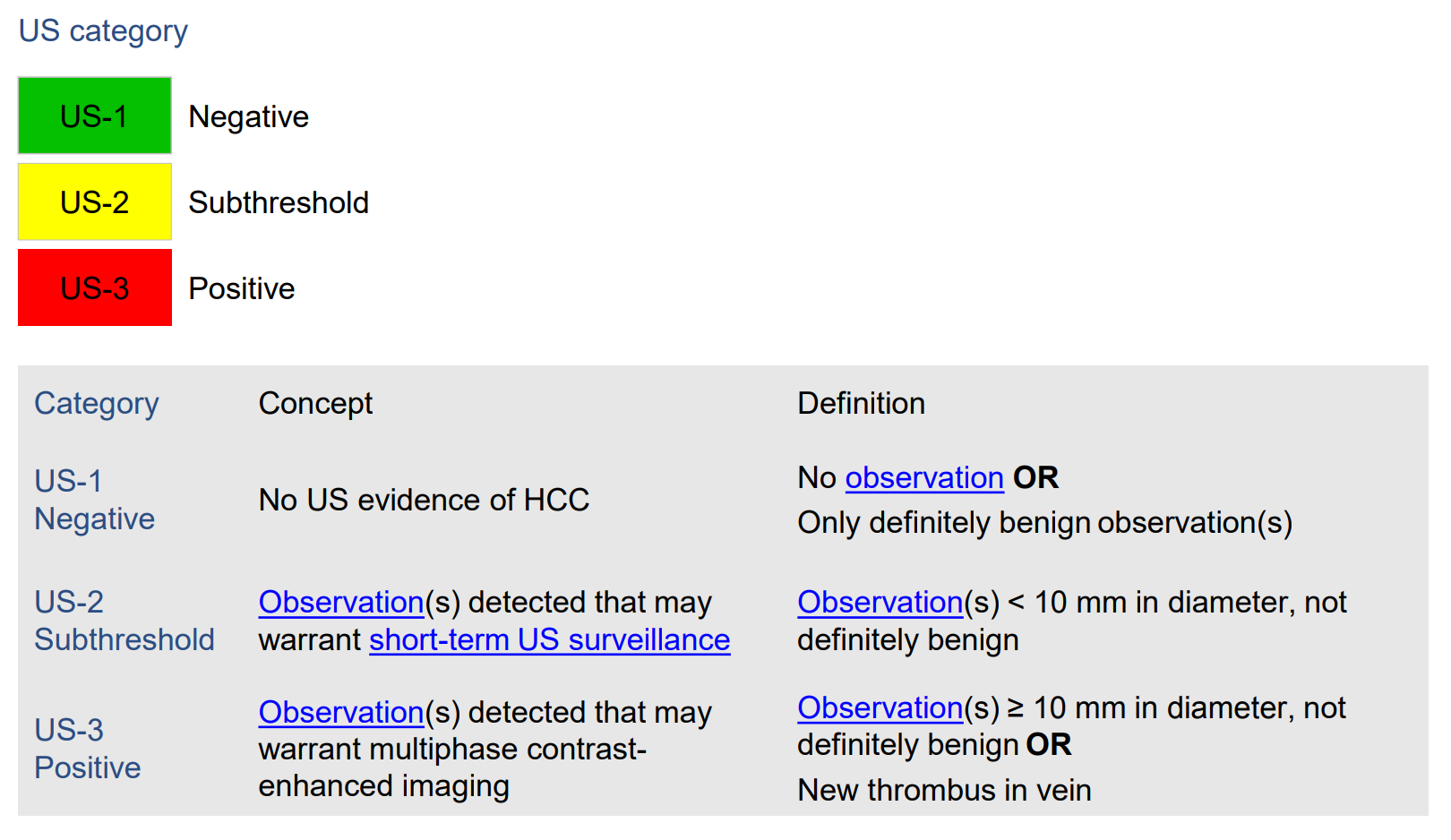
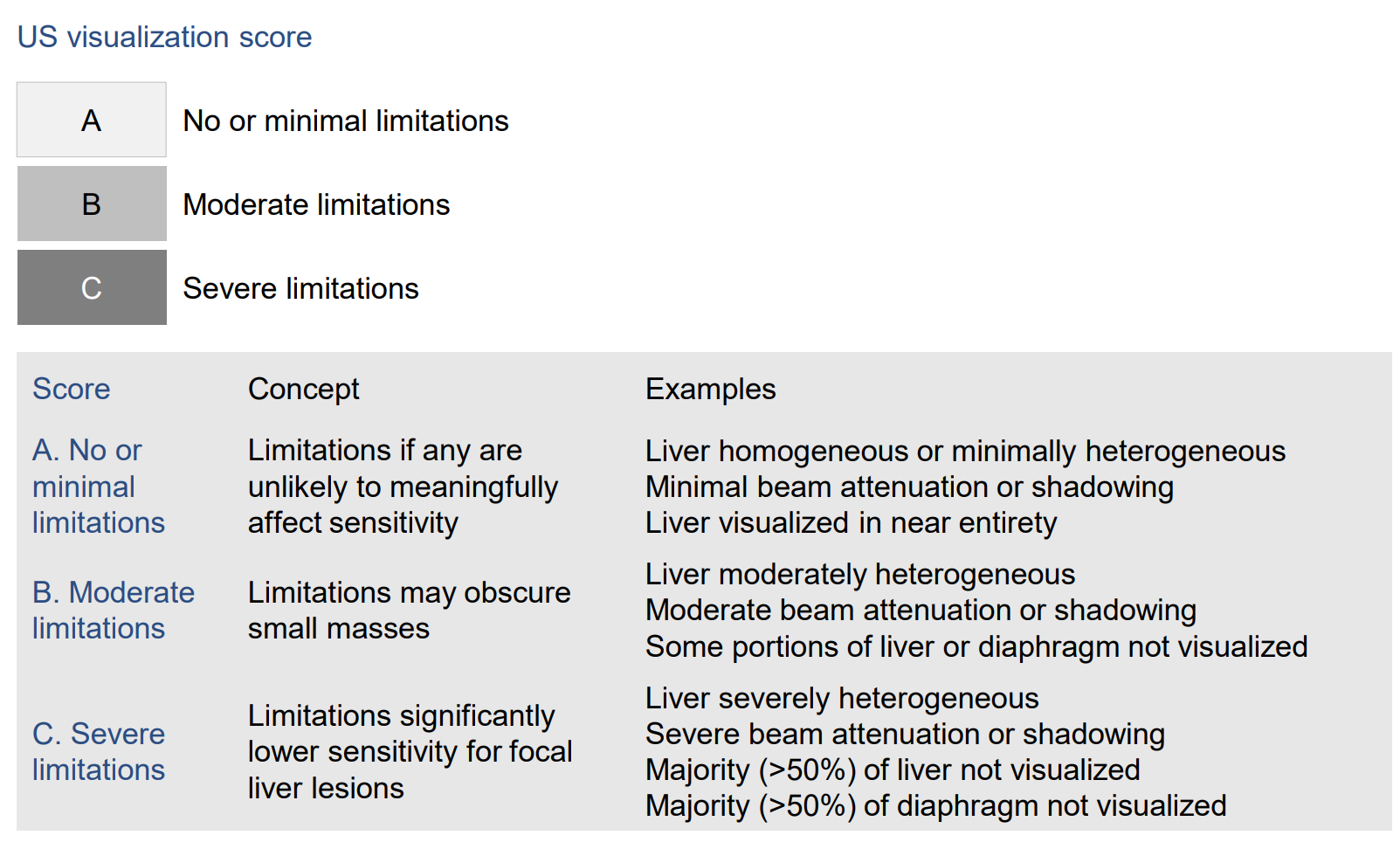
- Liver ACR
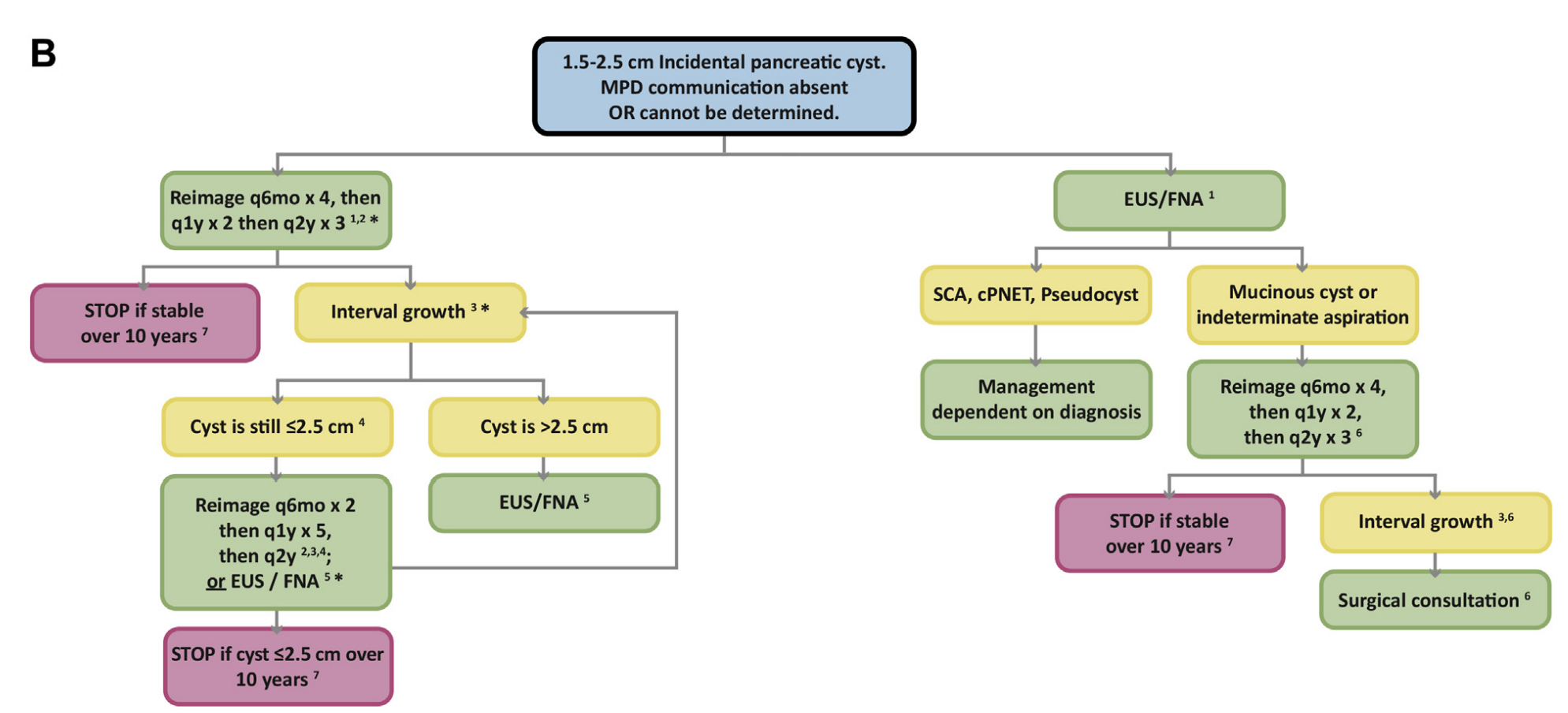
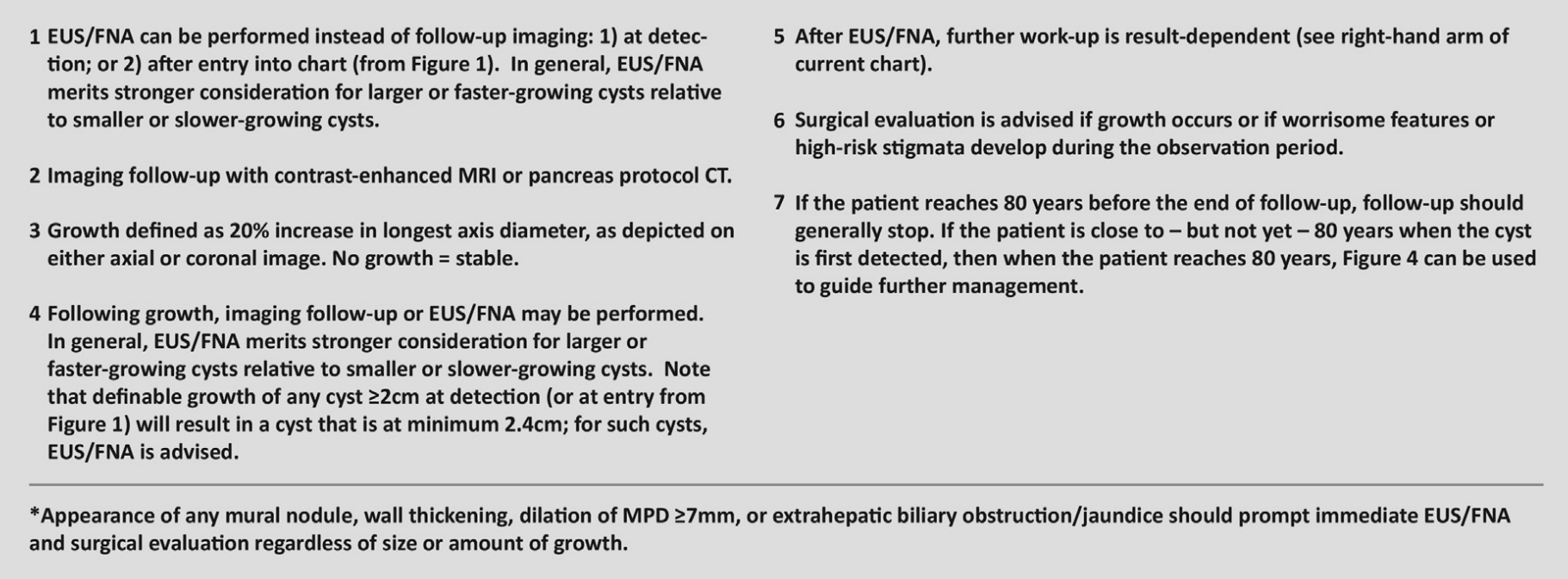
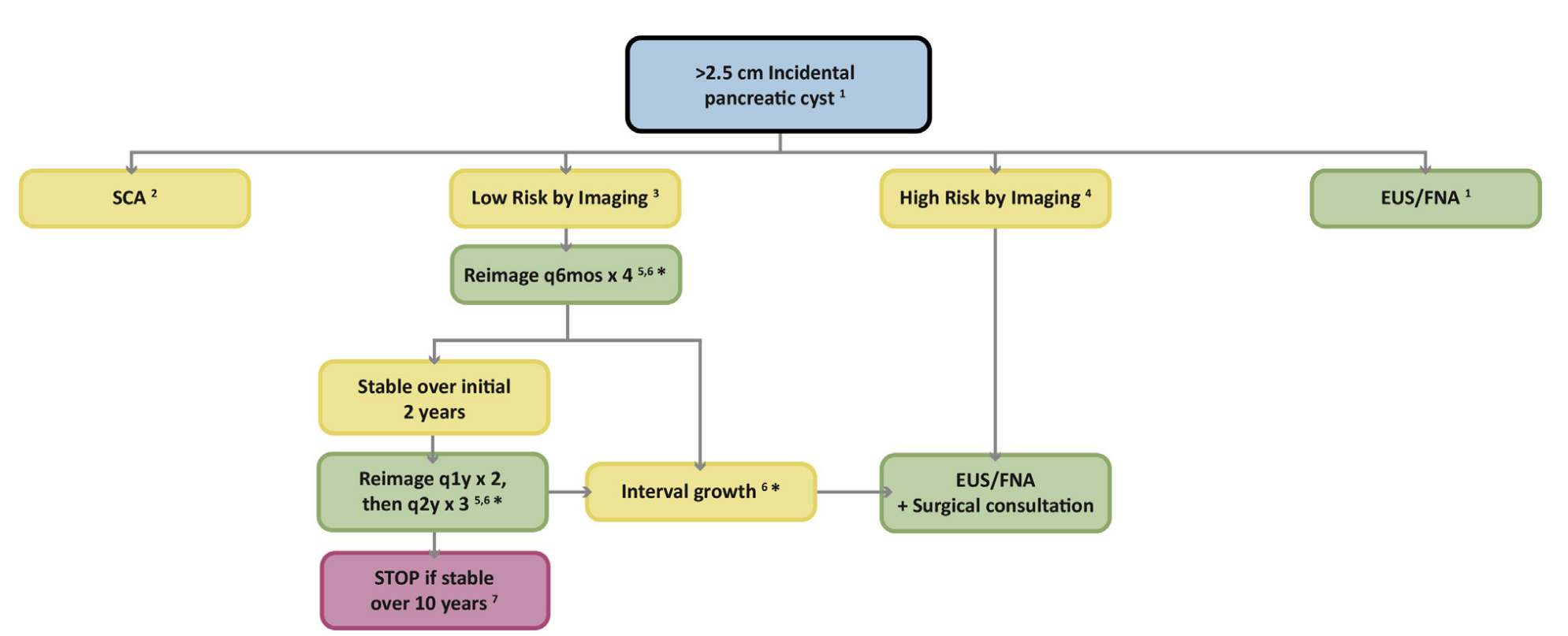
- Pancreas Cyst ACR
- Renal ACR
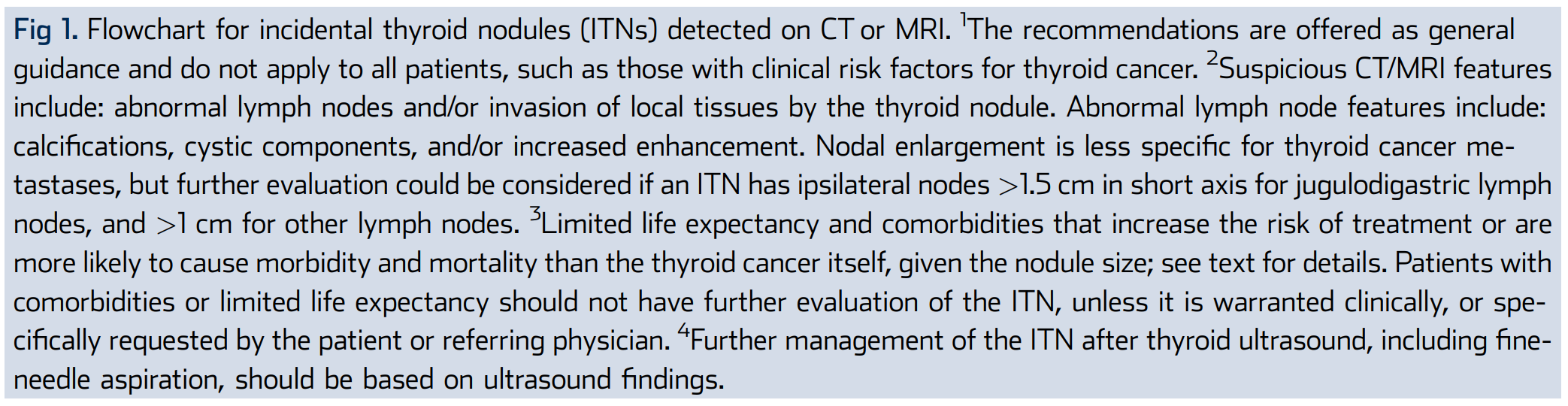
- Thyroid ACR





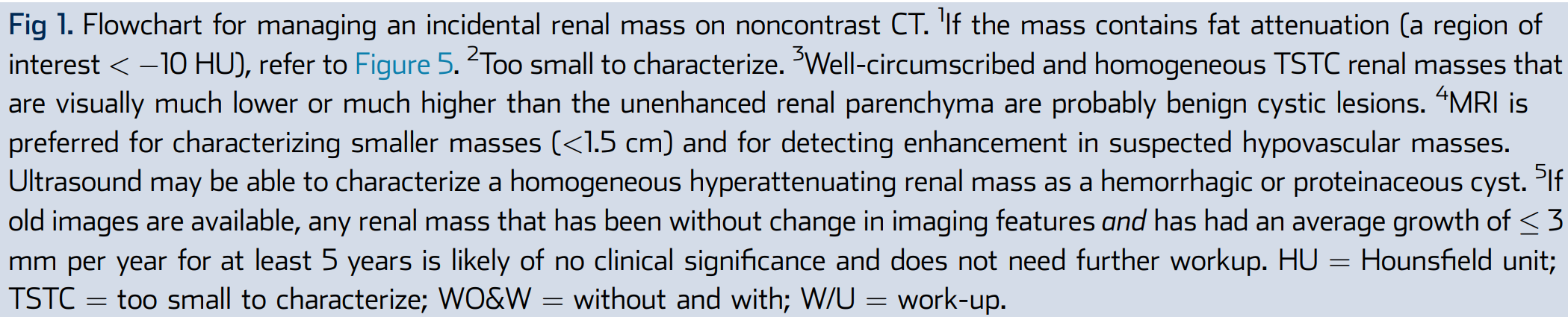
Non-contrast CT

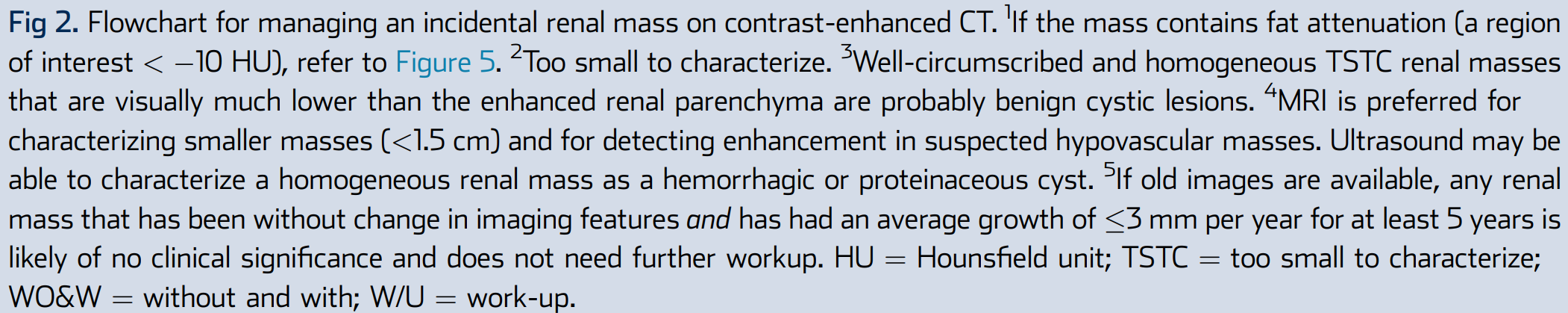
Contrast-enhanced CT


Incidental Cystic


Too Small to Characterize


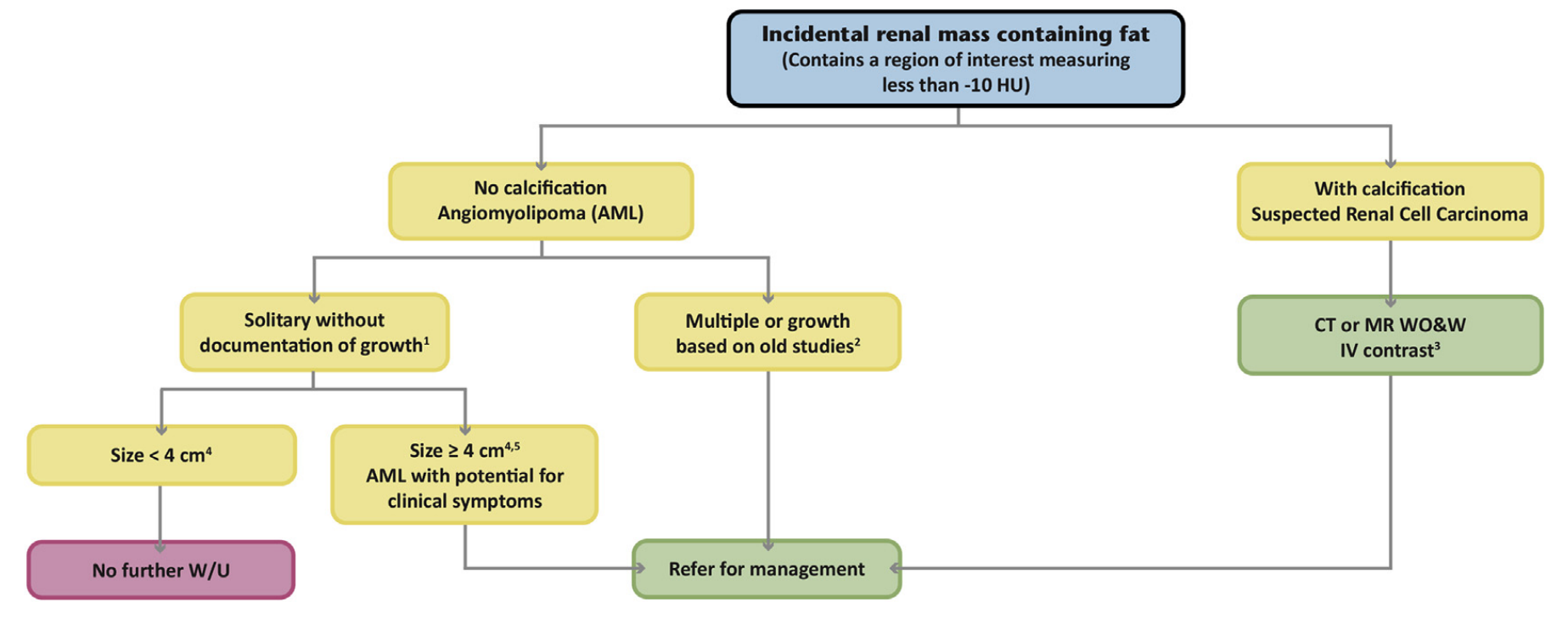
Containing Fat

Bosniak

- DWI and T2 Timing
- Vascular Territories
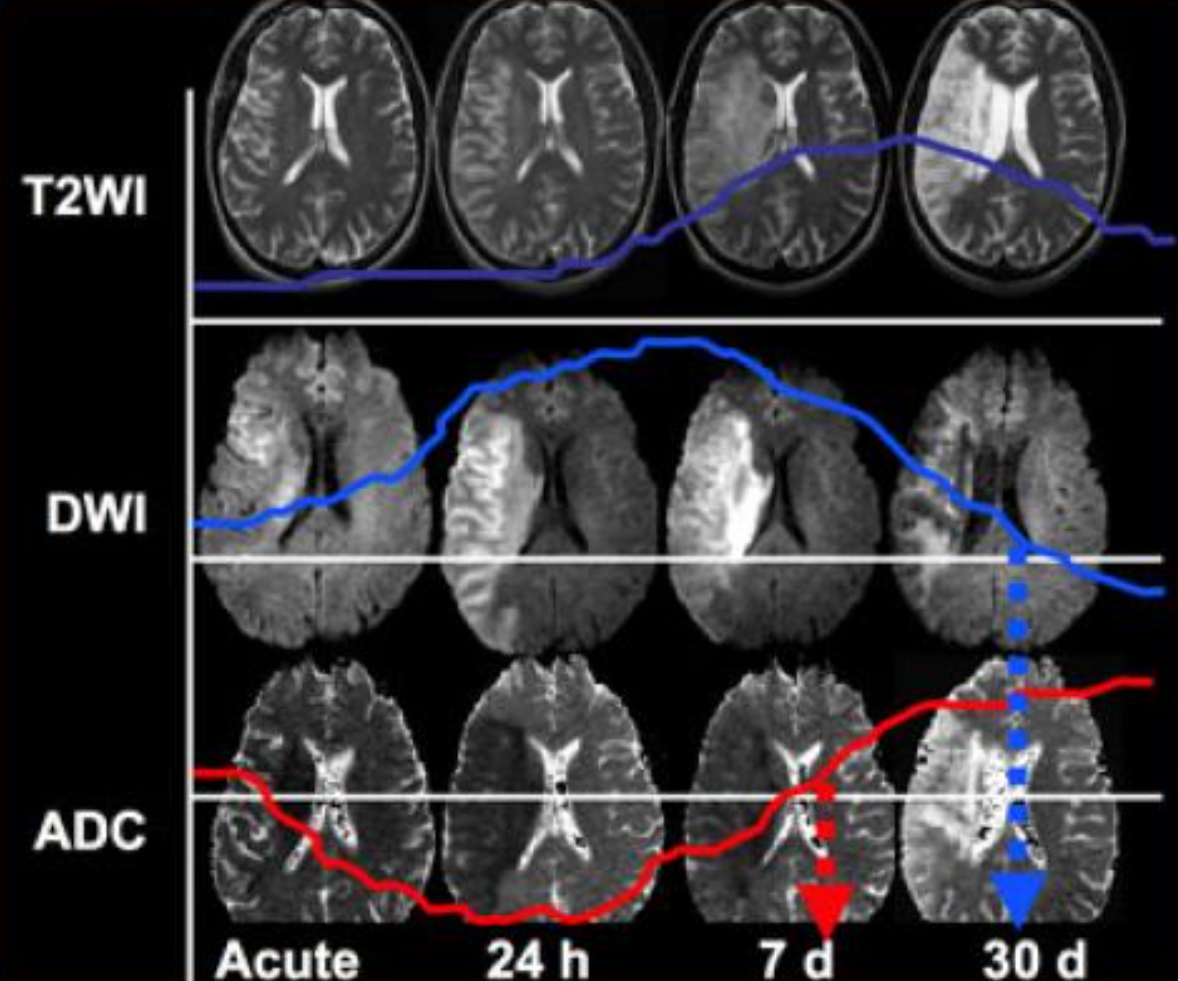
When we compare the findings on T2WI and DWI in time we will notice the following:
- In the acute phase T2WI will be normal, but in time the infarcted area will become hyperintense.
- The hyperintensity on T2WI reaches its maximum between 7 and 30 days. After this it starts to fade.
- DWI is already positive in the acute phase and then becomes more bright with a maximum at 7 days.
- DWI in brain infarction will be positive for approximately for 3 weeks after onset (in spinal cord infarction DWI is only positive for one week!).
- ADC will be of low signal intensity with a maximum at 24 hours and then will increase in signal intensity and finally becomes bright in the chronic stage.

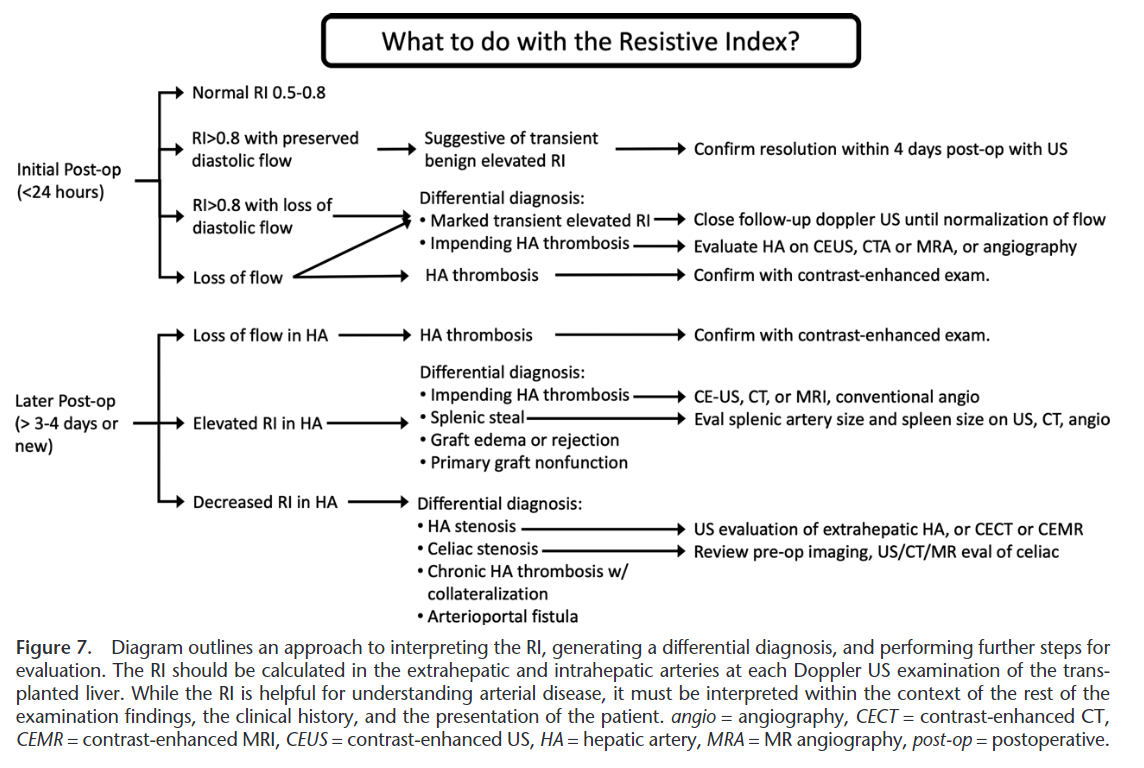
- Liver Resistive Index
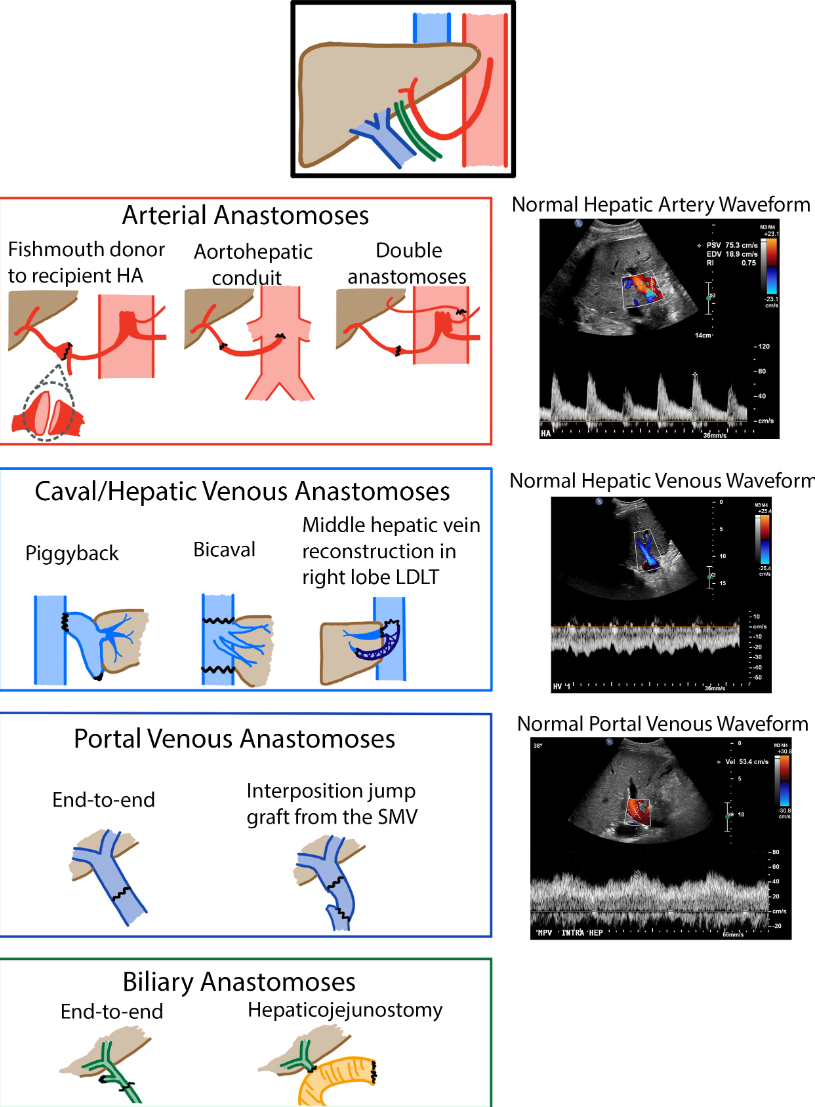
- Liver Tx Anatomy
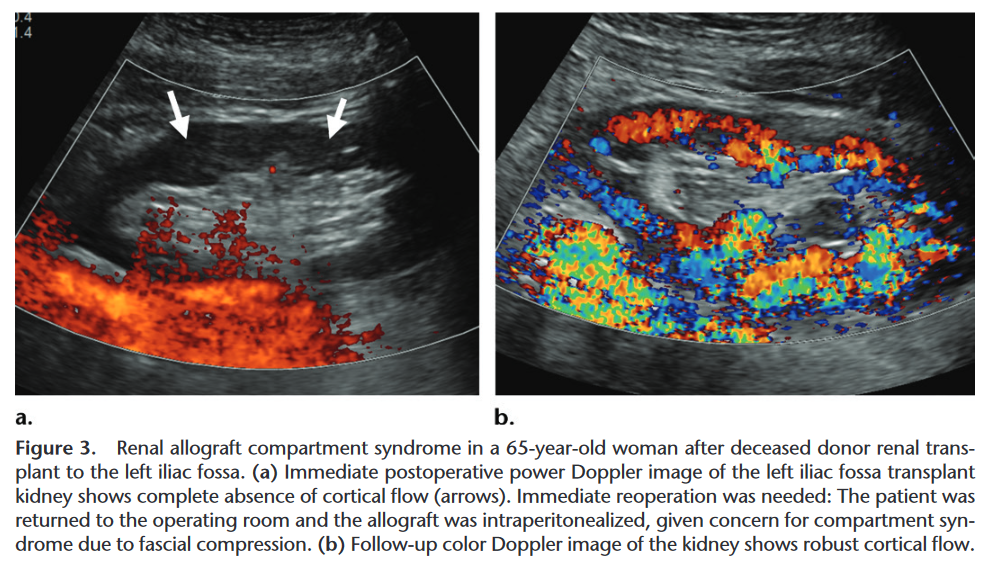
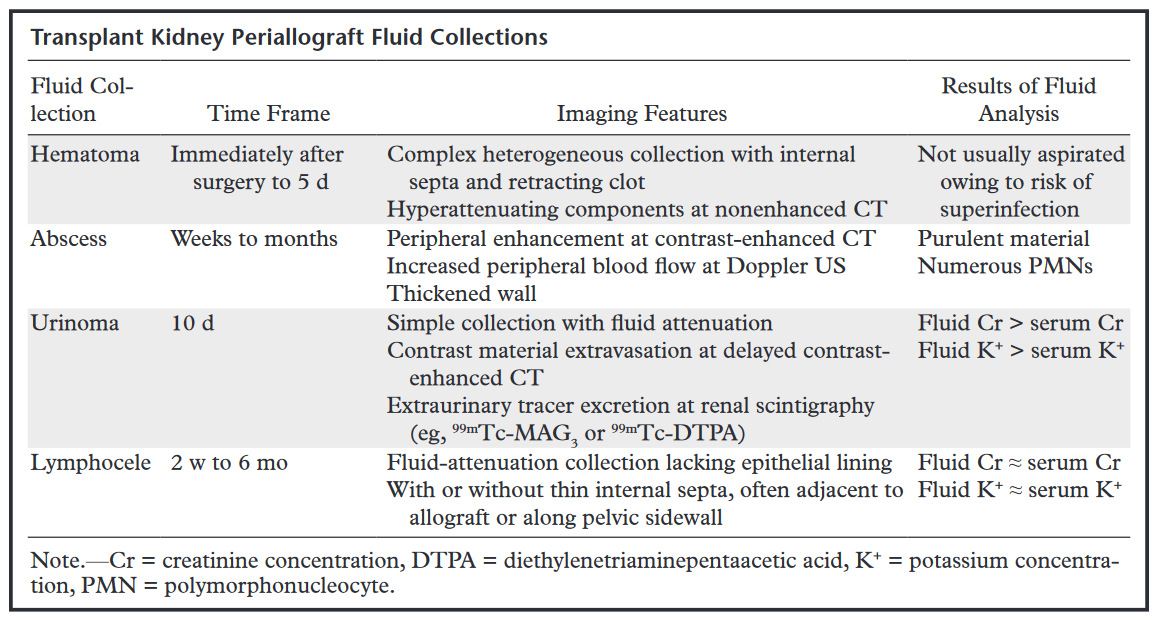
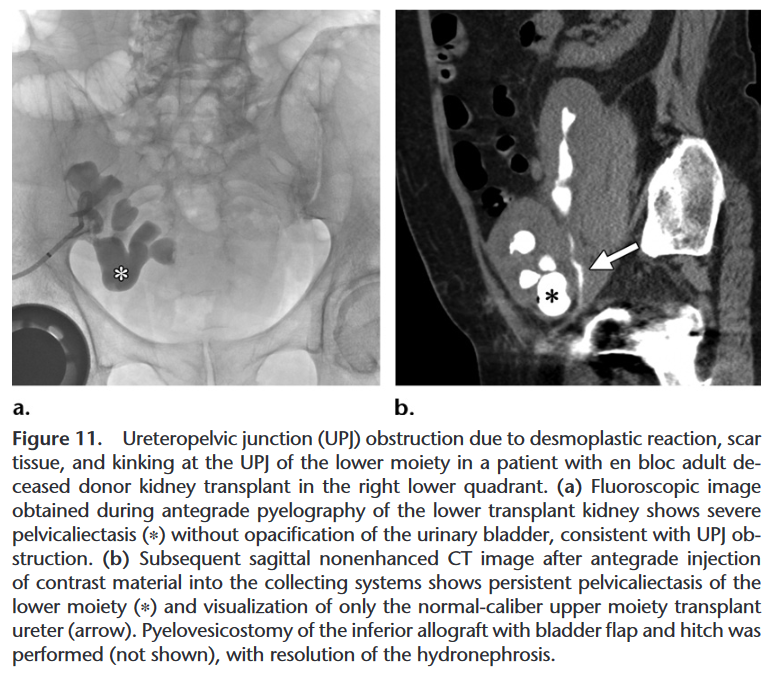
- Renal Transplant Complications




- Kidney AAST
- Liver AAST
- Spleen AAST

Kidney Injury Scale (2018 revision)
AAST Grade AIS Severity Imaging Criteria (CT Findings) Operative Criteria Pathologic Criteria I 2 Subcapsular hematoma and/or parenchymal
contusion without lacerationNonexpanding subcapsular hematoma Subcapsular hematoma or parenchymal
contusion without parenchymal laceration Parenchymal contusion without laceration II 2 Perirenal hematoma confined to Gerota fascia Nonexpanding perirenal hematoma
confined to Gerota fasciaPerirenal hematoma confined to
Gerota fascia Renal parenchymal laceration ≤1 cm depth
without urinary extravasationRenal parenchymal laceration ≤1 cm depth
without urinary extravasationRenal parenchymal laceration ≤1 cm
depth without urinary extravasation III 3 Renal parenchymal laceration >1 cm depth without
collecting system rupture or urinary extravasationRenal parenchymal laceration >1 cm depth
without collecting system rupture or
urinary extravasationRenal parenchymal laceration >1 cm
depth without collecting system
rupture or urinary extravasation Any injury in the presence of a kidney vascular injury
or active bleeding contained within Gerota fascia IV 4 Parenchymal laceration extending into urinary
collecting system with urinary extravasationParenchymal laceration extending into urinary
collecting system with urinary extravasationParenchymal laceration extending into urinary
collecting system Renal pelvis laceration and/or complete
ureteropelvic disruptionRenal pelvis laceration and/or complete
ureteropelvic disruptionRenal pelvis laceration and/or complete
ureteropelvic disruption Segmental renal vein or artery injury Segmental renal vein or artery injury Segmental renal vein or artery injury Active bleeding beyond Gerota fascia into the
retroperitoneum or peritoneumSegmental or complete kidney infarction(s)
due to vessel thrombosis without active bleedingSegmental or complete kidney infarction(s)
due to vessel thrombosis without active bleeding Segmental or complete kidney infarction(s)
due to vessel thrombosis without active bleeding V 5 Main renal artery or vein laceration or
avulsion of hilumMain renal artery or vein laceration or
avulsion of hilumMain renal artery or vein laceration or
avulsion of hilum Devascularized kidney with active bleeding Devascularized kidney with active bleeding Devascularized kidney Shattered kidney with loss of identifiable
parenchymal renal anatomyShattered kidney with loss of identifiable
parenchymal renal anatomyShattered kidney with loss of identifiable
parenchymal renal anatomyVascular injury is defined as a pseudoaneurysm or arteriovenous fistula and appears as a focal collection of vascular contrast that decreases in attenuation with delayed imaging. Active bleeding from a vascular injury presents as vascular contrast, focal or diffuse, that increases in size or attenuation in delayed phase. Vascular thrombosis can lead to organ infarction.
Grade based on highest grade assessment made on imaging, at operation or on pathologic specimen.
More than one grade of kidney injury may be present and should be classified by the higher grade of injury.
Advance one grade for multiple injuries up to grade III.

Liver Injury Scale (2018 revision)
AAST Grade AIS Severity Imaging Criteria (CT Findings) Operative Criteria Pathologic Criteria I 2 Subcapsular hematoma <10% surface area Subcapsular hematoma <10% surface area Subcapsular hematoma <10% surface area Parenchymal laceration <1 cm depth Parenchymal laceration <1 cm depth Parenchymal laceration <1 cm depth Capsular tear Capsular tear II 2 Subcapsular hematoma 10-50% surface area; intraparenchymal hematoma <10 cm in diameter Subcapsular hematoma 10-50% surface area; intraparenchymal hematoma <10 cm in diameter Subcapsular hematoma 10-50% surface
area; intraparenchymal hematoma
<10 cm in diameter Laceration 1-3 cm in depth and
≤10 cm lengthLaceration 1-3 cm in depth and
≤10 cm lengthLaceration 1-3 cm in depth and
≤10 cm length III 3 Subcapsular hematoma >50% surface area;
ruptured subcapsular or parenchymal
hematoma Subcapsular hematoma >50% surface area or
expanding; ruptured subcapsular or
parenchymal hematomaSubcapsular hematoma >50% surface area;
ruptured subcapsular or intraparenchymal
hematoma Intrparenchymal laceration >10 cm Intraparenchymal hematoma >10 cm Intraparenchymal hematoma >10 cm Laceration >3 cm depth Laceration >3 cm depth Laceration >3 cm depth Any injury in the presence of a liver
vascular injury or active bleeding
contained within liver parenchyma IV 4 Parenchymal disruption involving
25-75% of a hepatic lobeParenchymal disruption involving
25-75% of a hepatic lobeParenchymal disruption involving
25-75% of a hepatic lobe Active bleeding extending beyond the
liver parenchyma into the peritoneum V 5 Parenchymal disruption >75% of hepatic lobe Parenchymal disruption >75% of hepatic lobe Parenchymal disruption >75% of hepatic lobe Juxtahepatic venous injury to include
retrohepatic vena cava and central
major hepatic veinsJuxtahepatic venous injury to include
retrohepatic vena cava and central
major hepatic veinsJuxtahepatic venous injury to include
retrohepatic vena cava and central
major hepatic veinsVascular injury is defined as a pseudoaneurysm or arteriovenous fistula and appears as a focal collection of vascular contrast that decreases in attenuation with delayed imaging. Active bleeding from a vascular injury presents as vascular contrast, focal or diffuse, that increases in size or attenuation in delayed phase. Vascular thrombosis can lead to organ infarction.
Grade based on highest grade assessment made on imaging, at operation or on pathologic specimen.
More than one grade of liver injury may be present and should be classified by the higher grade of injury.
Advance one grade for multiple injuries up to grade III.

Vascular injury is defined as a pseudoaneurysm or arteriovenous fistula and appears as a focal collection of vascular contrast that decreases in attenuation with delayed imaging. Active bleeding from a vascular injury presents as vascular contrast, focal or diffuse, that increases in size or attenuation in delayed phase. Vascular thrombosis can lead to organ infarction. From Kozar et al.; with permissionSpleen Injury Scale (2018 revision)
Grade* AIS Severity Imaging Criteria (CT Findings) Operative Criteria Pathologic Criteria I 2 Subcapsular hematoma <10% surface area Subcapsular hematoma <10% surface area Subcapsular hematoma <10% surface area Parenchymal laceration <1 cm depth Parenchymal laceration <1 cm depth Parenchymal laceration <1 cm depth Capsular tear Capsular tear Capsular tear II 2 Subcapsular hematoma 10-50% surface
area; intraparenchymal hematoma <5 cmSubcapsular hematoma 10-50% surface
area; intraparenchymal hematoma <5 cmSubcapsular hematoma 10-50% surface
area; intraparenchymal hematoma <5 cm Parenchymal laceration 1-3 cm Parenchymal laceration 1-3 cm Parenchymal laceration 1-3 cm III 3 Subcapsular hematoma >50% surface area;
ruptured subcapsular or intraparenchymal
hematoma ≥5 cmSubcapsular hematoma >50% surface area or
expanding; ruptured subcapsular or
intraparenchymal hematoma ≥5 cmSubcapsular hematoma >50% surface area;
ruptured subcapsular or intraparenchymal
hematoma ≥5 cm Parenchymal laceration >3 cm depth Parenchymal laceration >3 cm depth Parenchymal laceration >3 cm depth IV 4 Any injury in the presence of a splenic
vascular injury or active bleeding confined
within splenic capsuleParenchymal laceration involving segmental or
hilar vessels producing >25% devascularizationParenchymal laceration involving segmental or
hilar vessels producing >25% devascularization Parenchymal laceration involving segmental or
hilar vessels producing >25% devascularization V 5 Any injury in the presence of a splenic vascular
injury with active bleeding extended beyond
the spleen into the peritoneumHilar vascular injury with devascularizes
the spleenHilar vascular injury with devascularizes
the spleen Shattered spleen Shattered spleen Shattered spleen
Grade based on highest grade assessment made on imaging, at operation or on pathologic specimen.
More than one grade of splenic injury may be present and should be classified by the higher grade of injury.
Advance one grade for multiple injuries up to grade III.
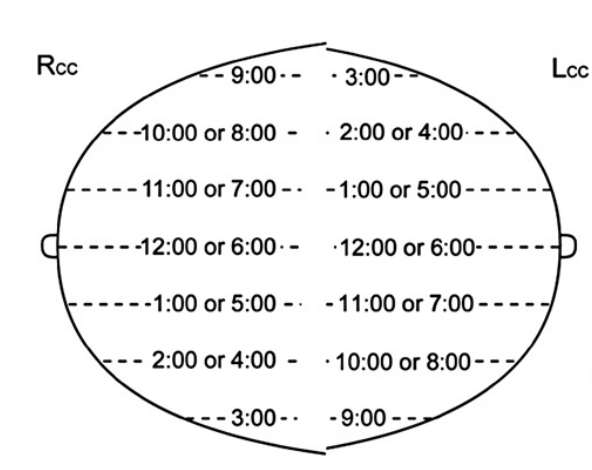
- Clock Face
- Density
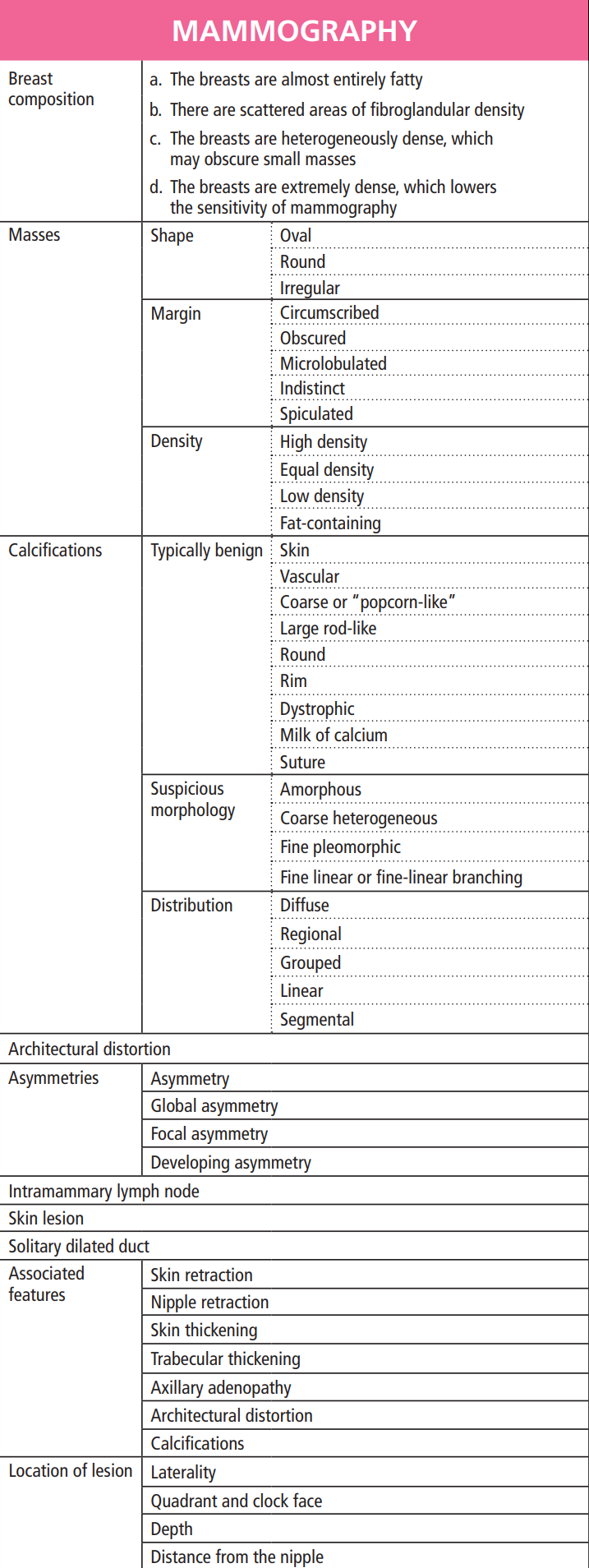
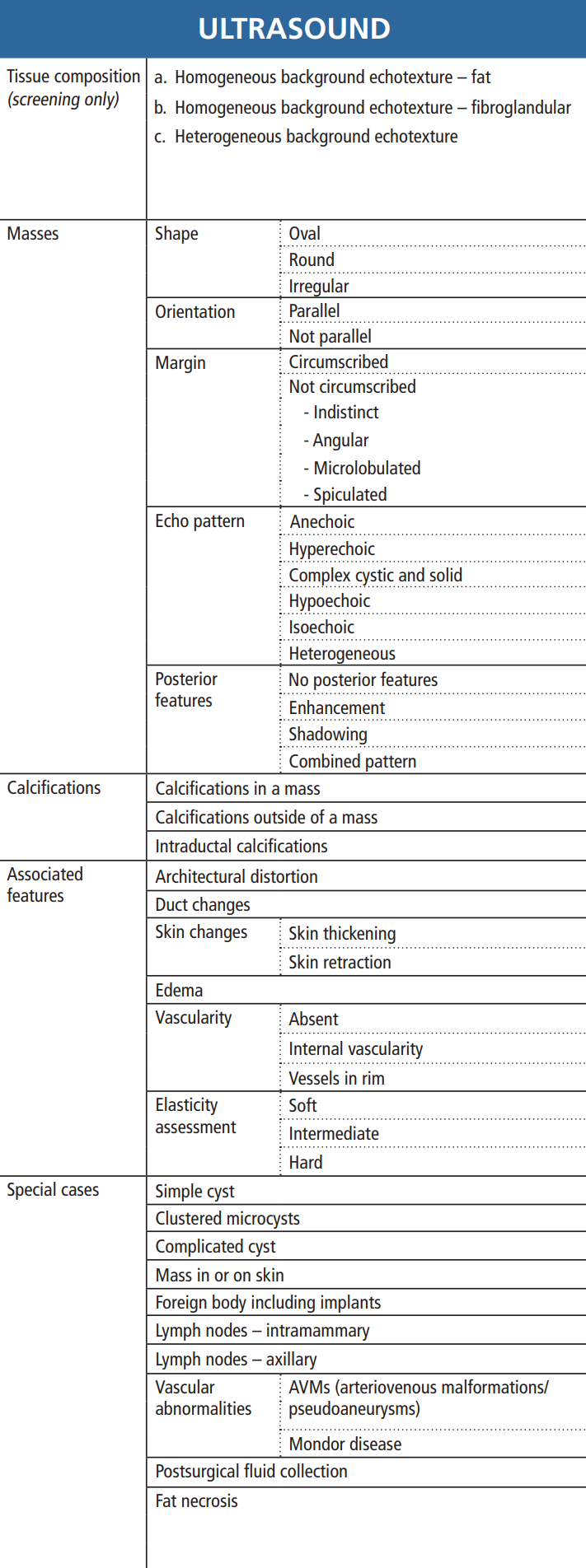
- Lexicon



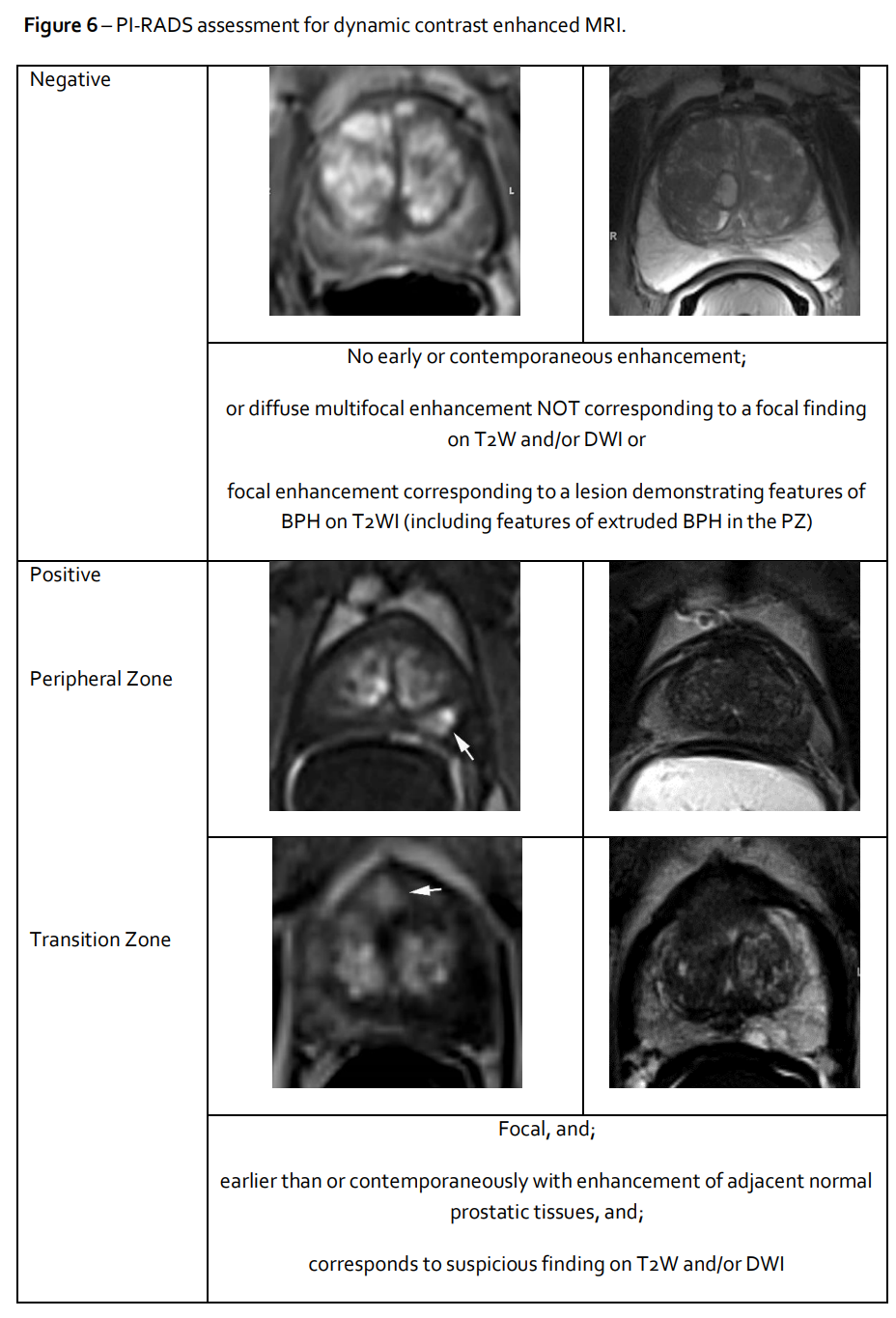
- DCE
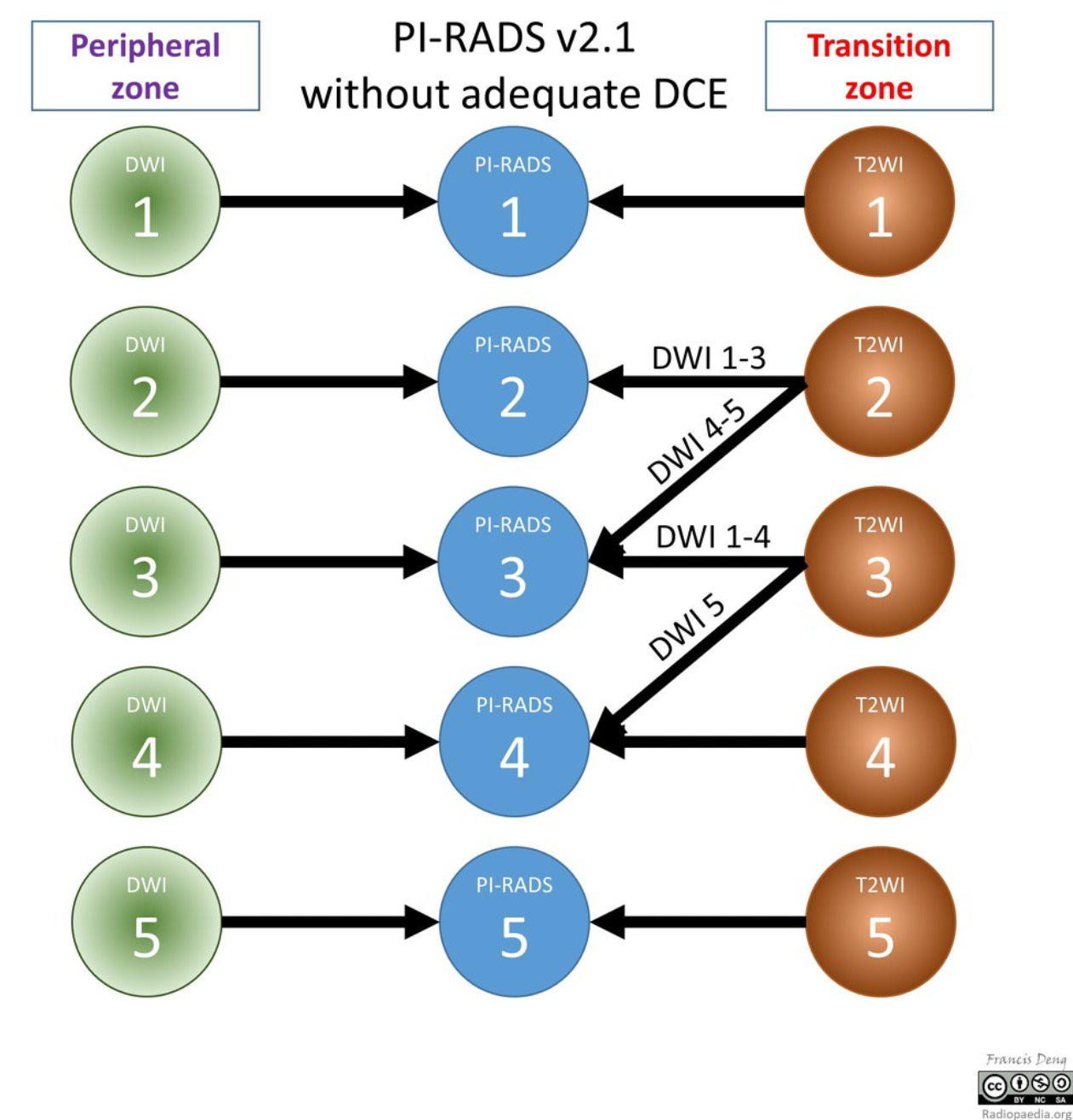
- DCE Inadequate
- DWI Inadequate
- Overview
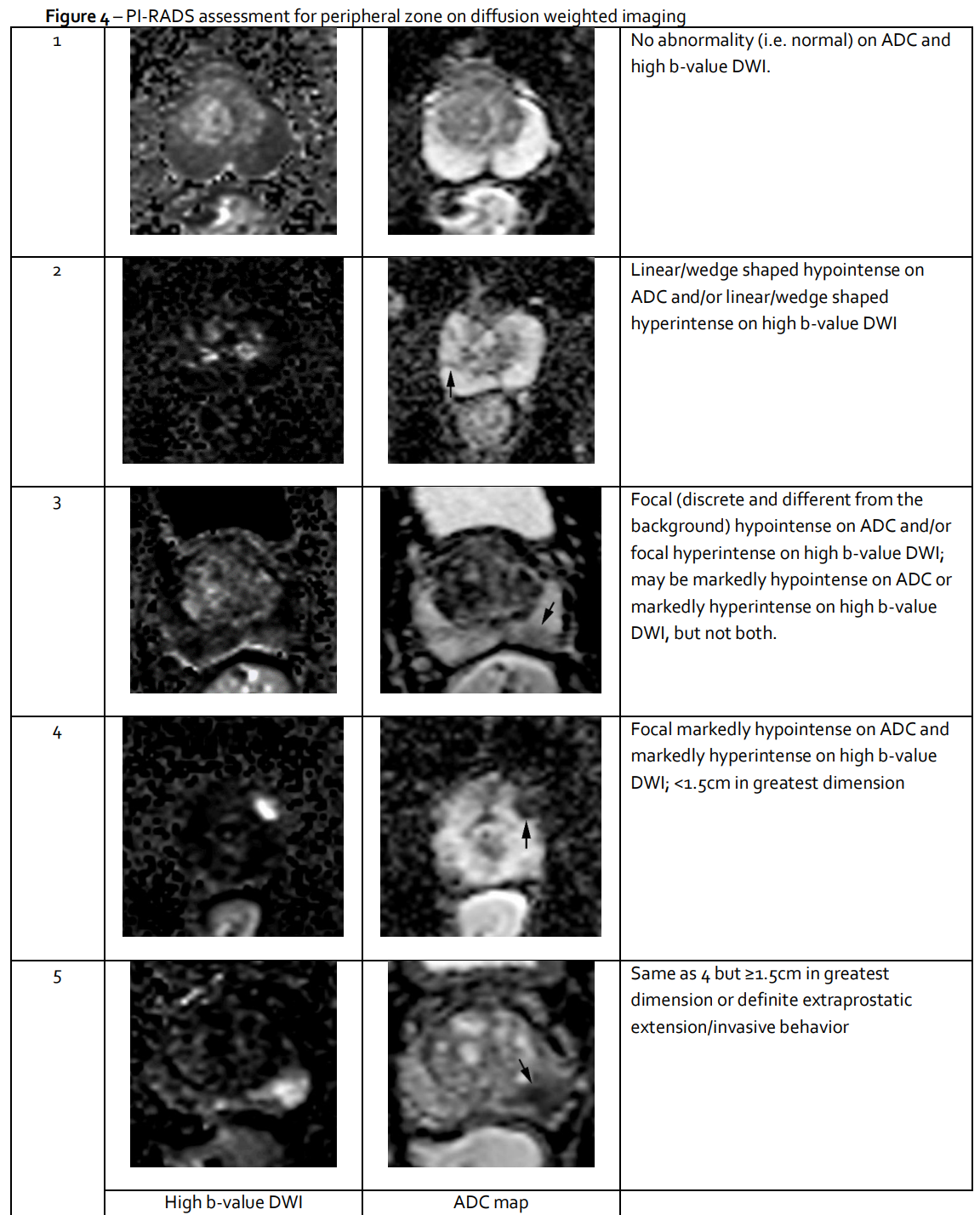
- Peripheral Zone DWI
- Peripheral Zone T2
- Transition Zone DWI
- Transition Zone T2





- Alternative Chart
- Chart
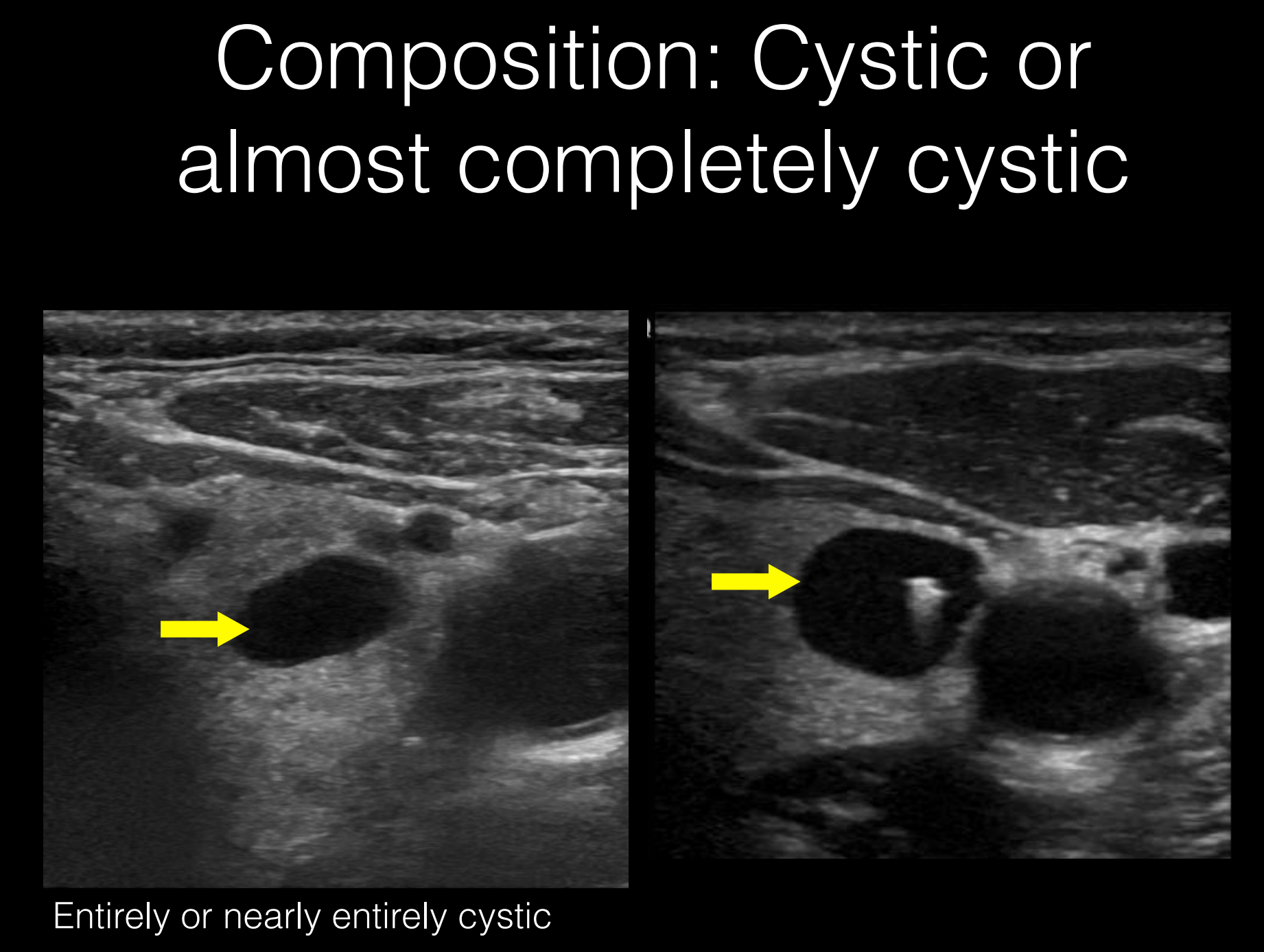
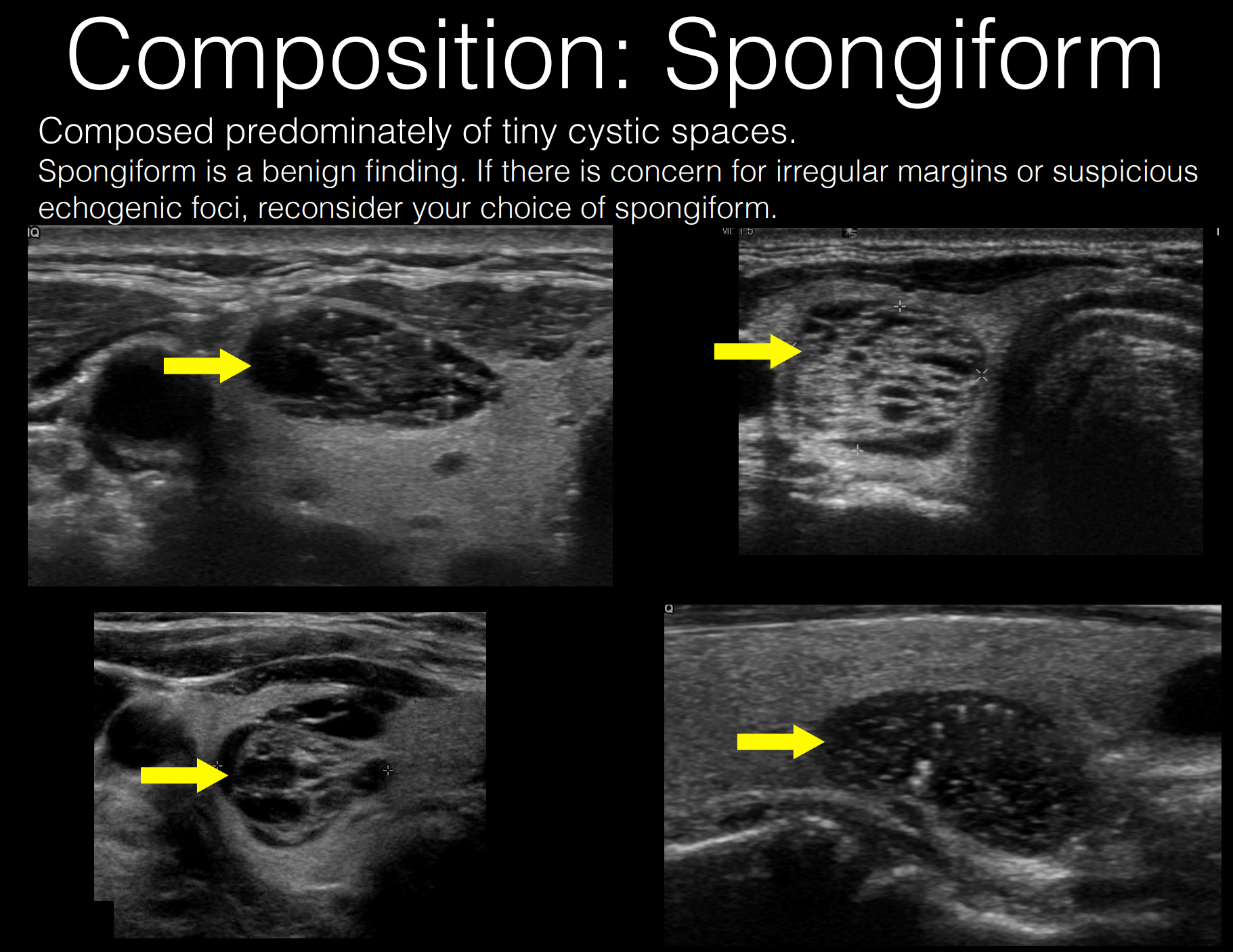
- Composition
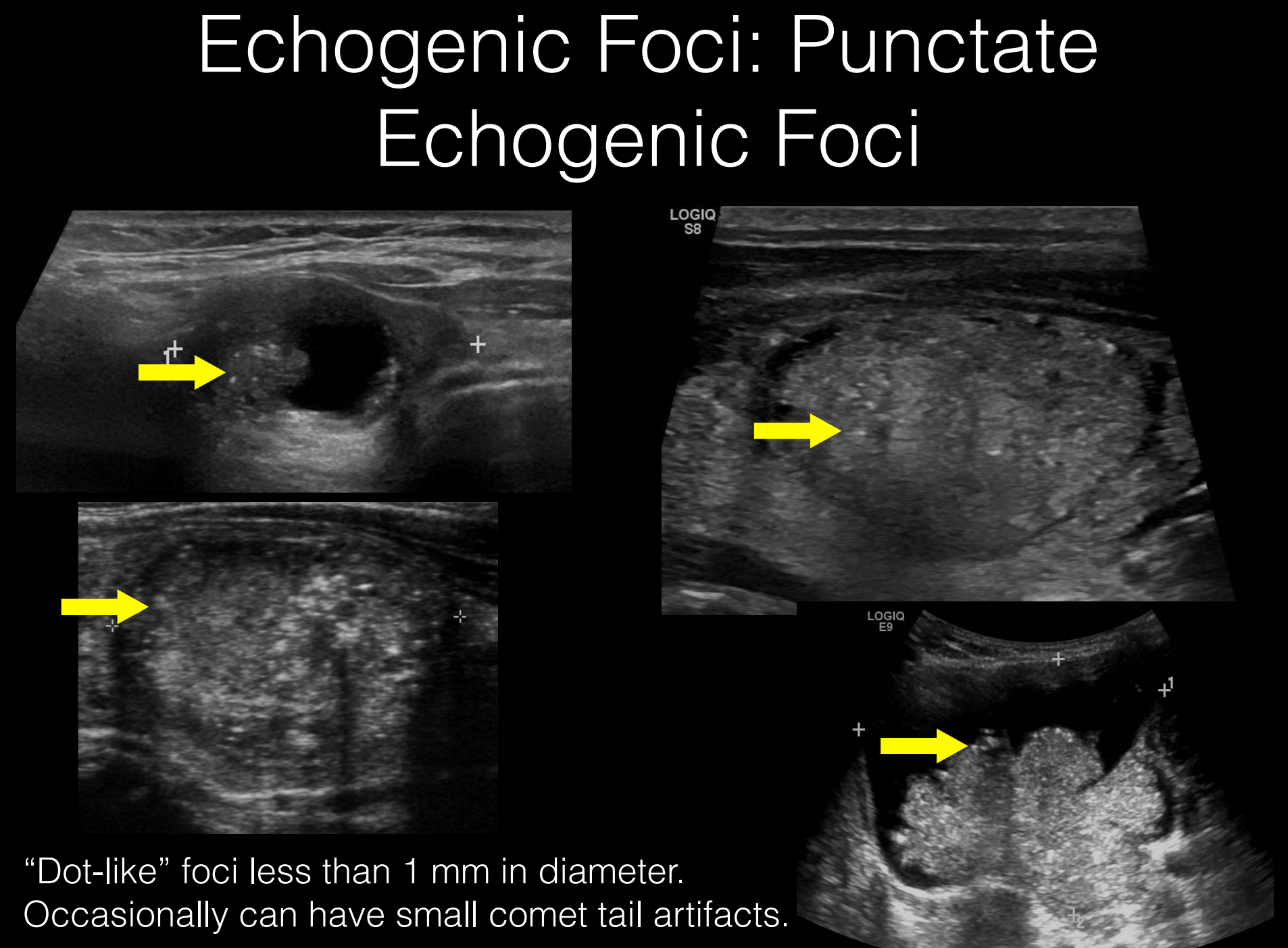
- Echogenic Foci
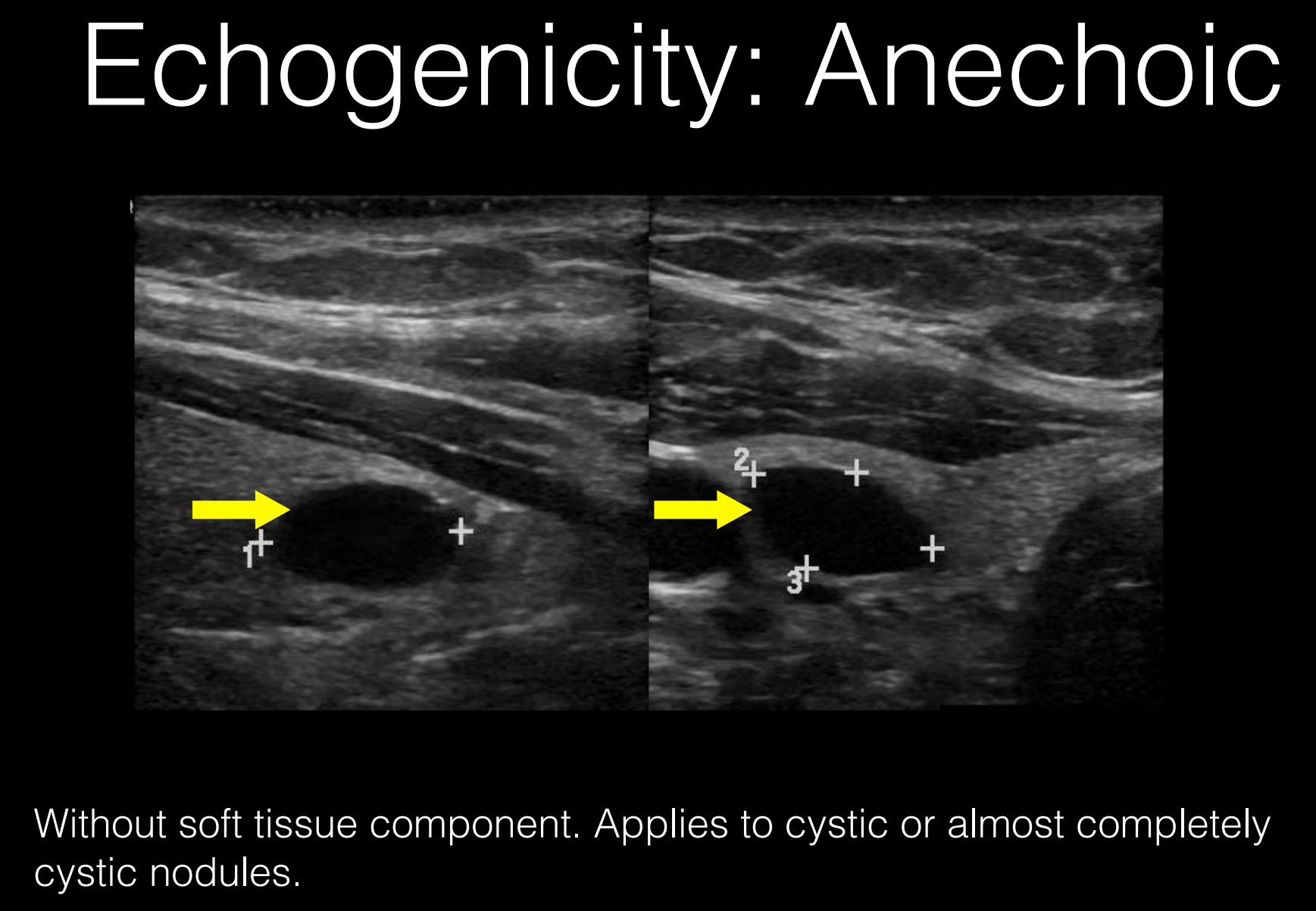
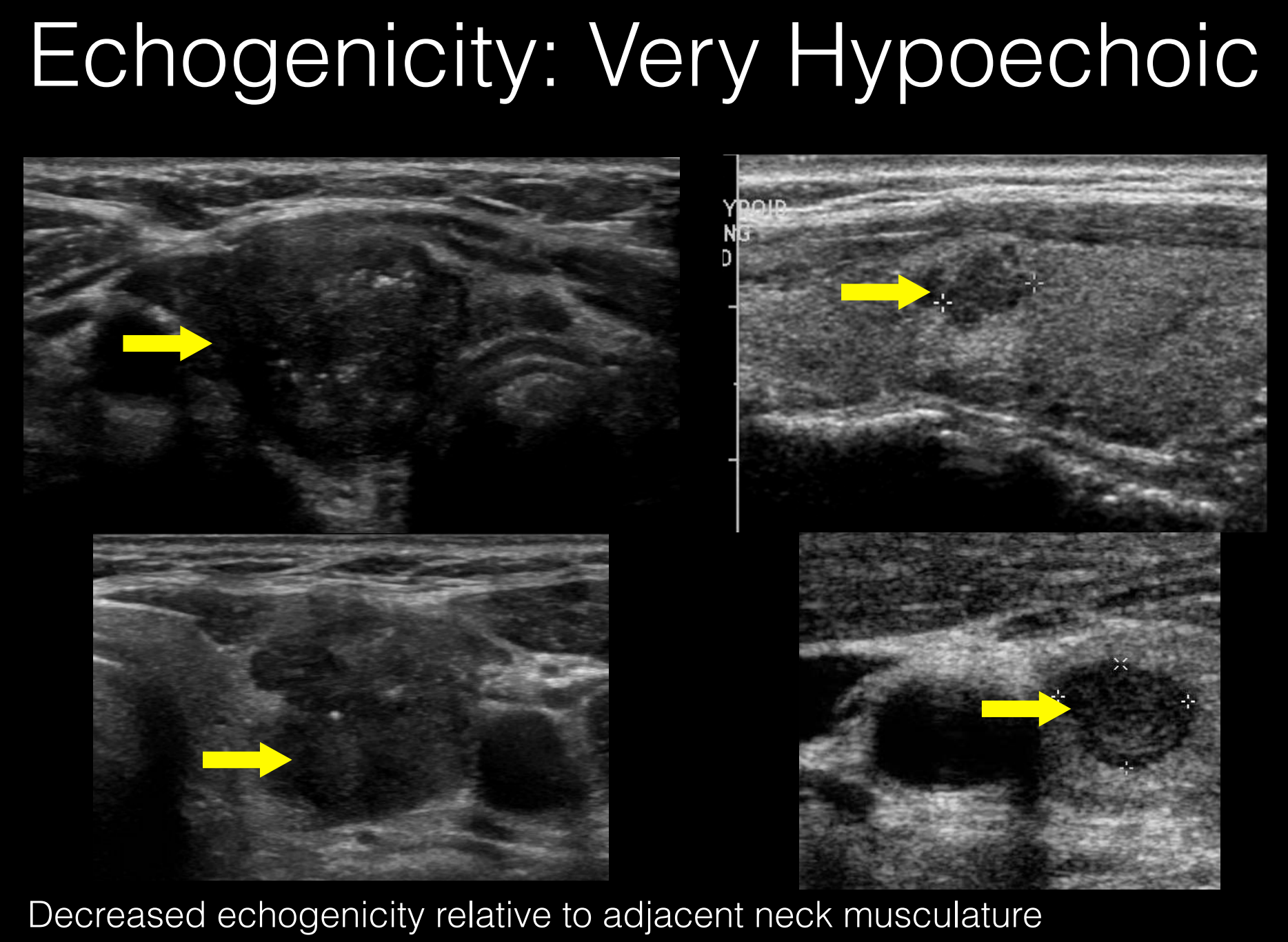
- Echogenicity
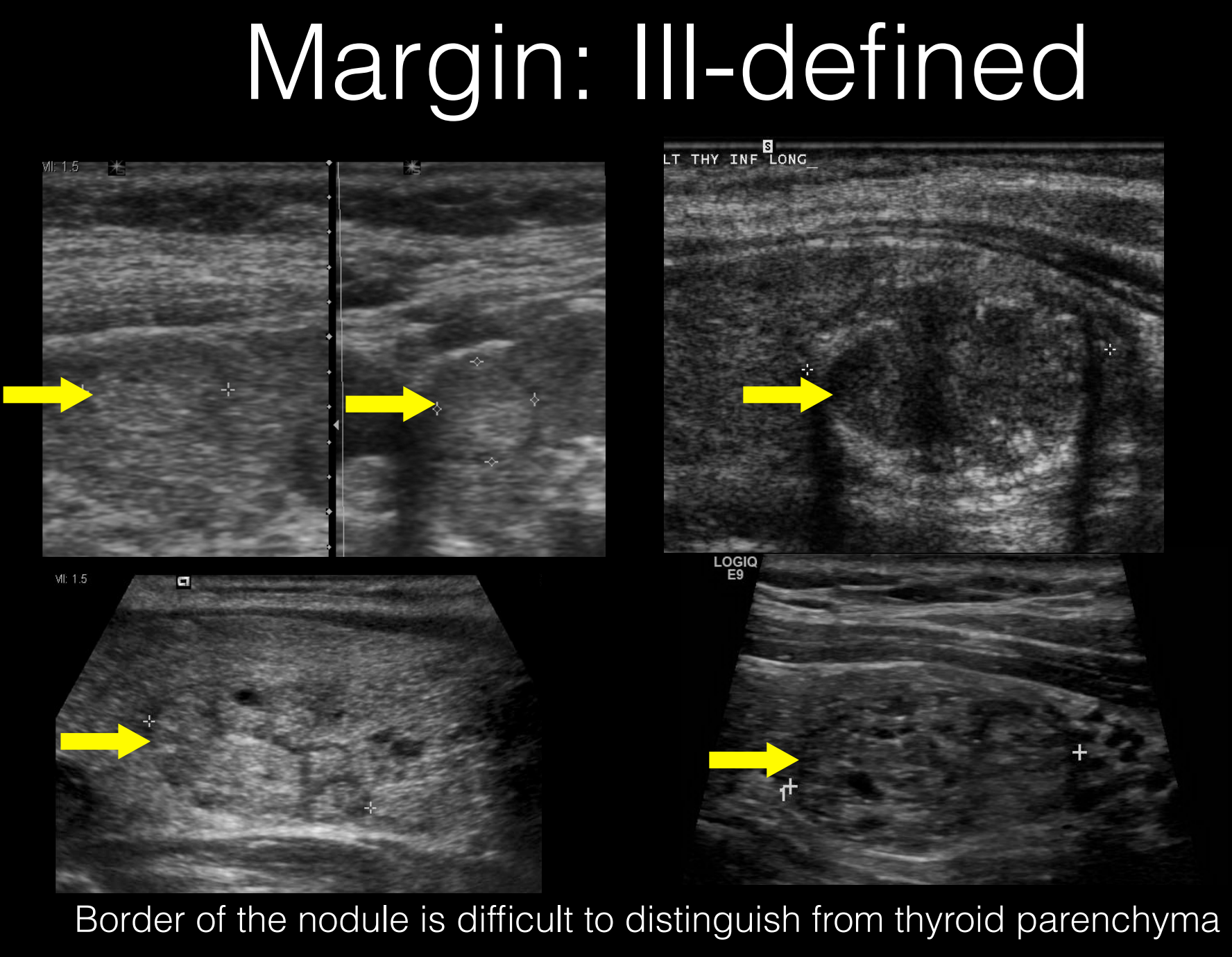
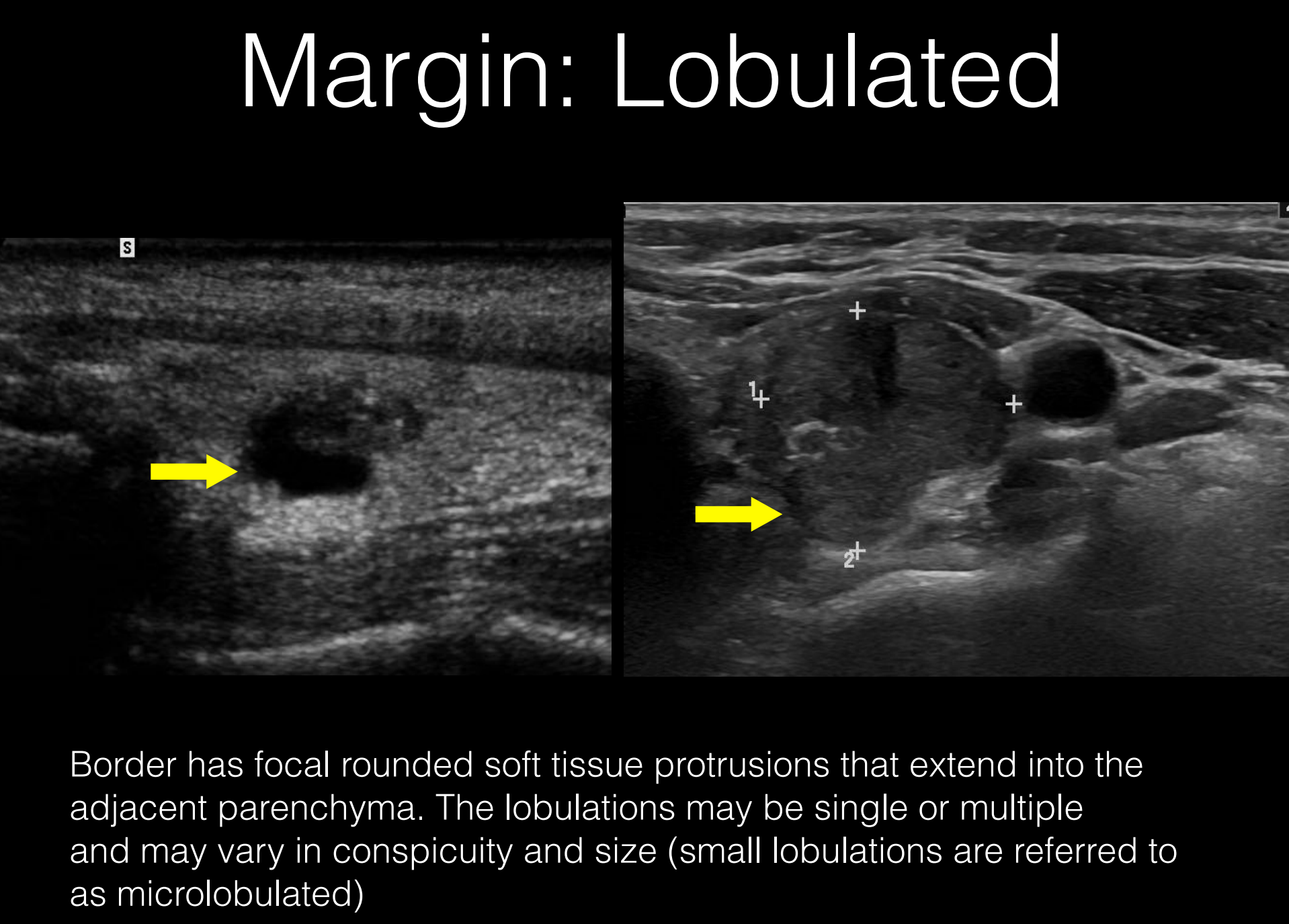
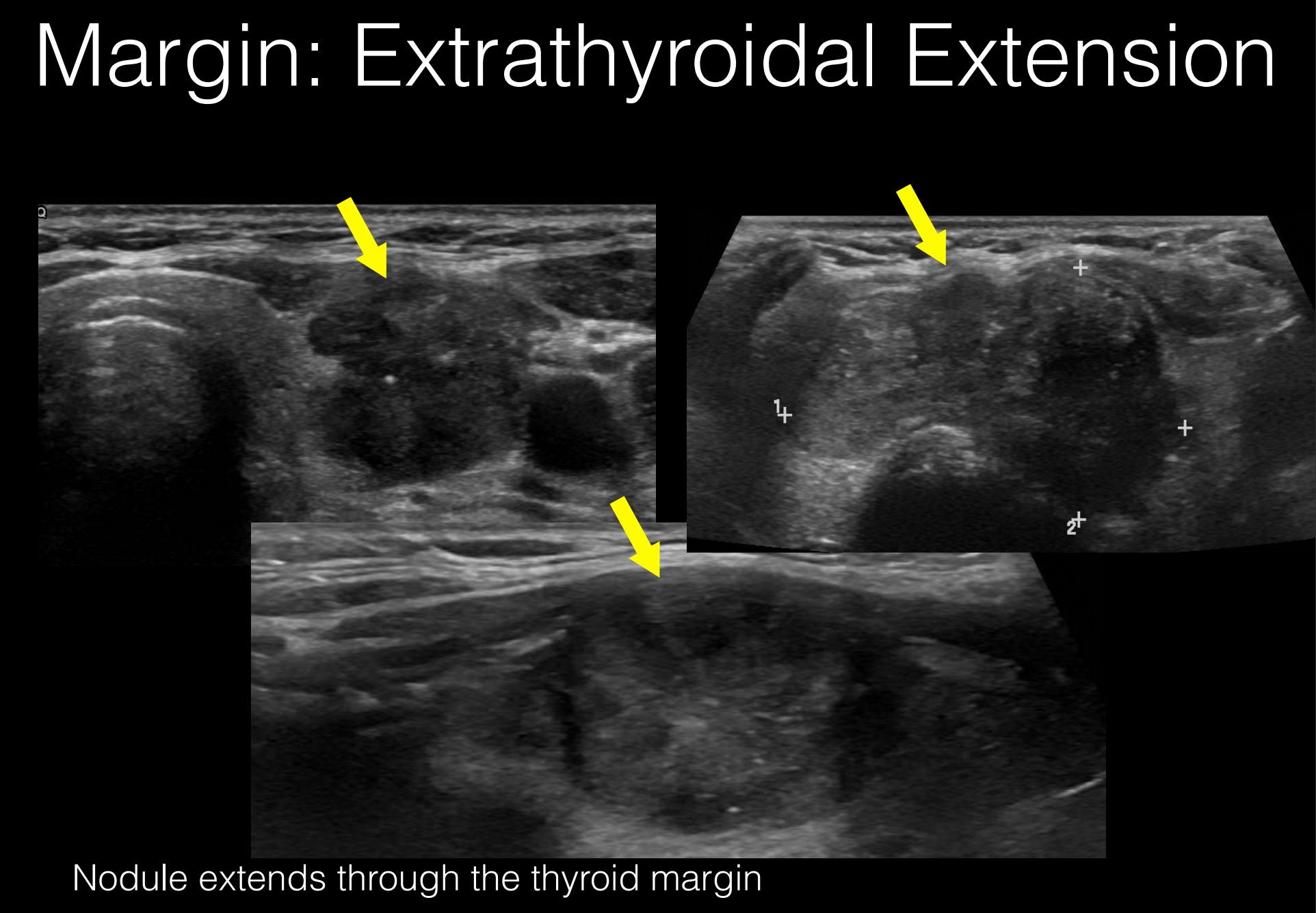
- Margin
- Shape